Seasonal influenza vaccination training 2 hrs – Commencing with “Seasonal Influenza Vaccination Training: A Comprehensive Guide,” this introductory paragraph captivates readers, setting the authoritative academic tone that will guide the discussion.
Influenza, a highly contagious respiratory illness, poses significant health risks, particularly during seasonal outbreaks. Vaccination remains the most effective preventive measure, and this training aims to equip healthcare professionals with the knowledge and skills necessary to administer seasonal influenza vaccines effectively.
Seasonal Influenza Vaccination Training: Seasonal Influenza Vaccination Training 2 Hrs

Seasonal influenza, a highly contagious respiratory illness, is a major public health concern worldwide. Vaccination is the most effective way to prevent influenza and its associated complications. This training aims to provide comprehensive knowledge and skills for healthcare professionals to effectively administer seasonal influenza vaccines.
Vaccine Components and Efficacy
Influenza vaccines contain inactivated or attenuated influenza viruses that stimulate the immune system to produce antibodies against the specific strains included in the vaccine. There are two main types of influenza vaccines:
- Inactivated influenza vaccine (IIV): Contains inactivated (killed) influenza viruses.
- Live attenuated influenza vaccine (LAIV): Contains weakened (attenuated) influenza viruses.
Both IIV and LAIV are effective in preventing influenza, but they have different efficacy rates and target populations.
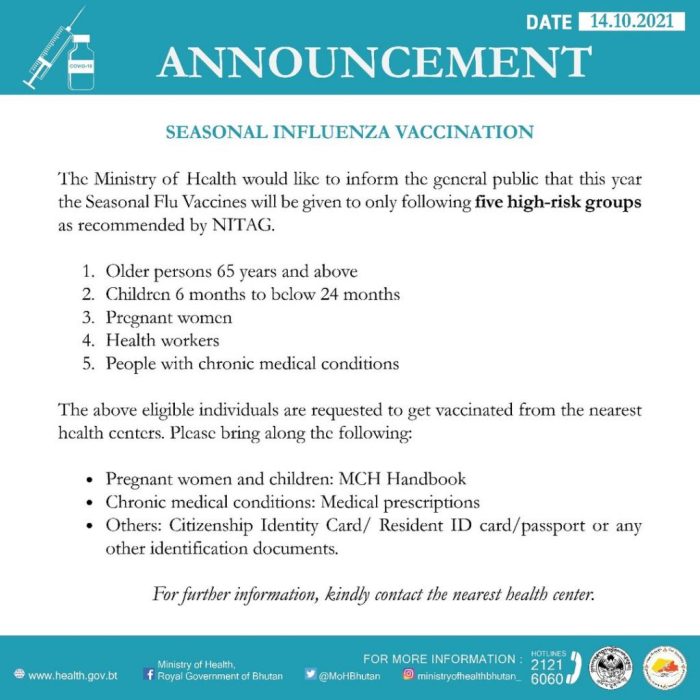
Target Population and Recommendations
The target population for seasonal influenza vaccination includes:
- Individuals at high risk of developing complications from influenza, such as the elderly, young children, pregnant women, and those with chronic health conditions.
- Healthcare workers and other individuals who are in close contact with high-risk populations.
- Individuals who live in congregate settings, such as nursing homes or dormitories.
The recommended schedule and frequency of vaccination vary depending on the vaccine type and the patient’s age and health status.
Administration and Storage
Influenza vaccines are typically administered intramuscularly (IM) in the deltoid muscle. Proper injection technique is essential to ensure vaccine effectiveness and minimize adverse reactions.
Influenza vaccines must be stored and handled according to the manufacturer’s instructions. Improper storage can compromise vaccine efficacy and safety.
Contraindications and Precautions
Contraindications to influenza vaccination include:
- Severe allergic reaction to a previous dose of influenza vaccine or any of its components.
- Guillain-Barré syndrome within 6 weeks of a previous dose of influenza vaccine.
Precautions should be taken in patients with certain medical conditions, such as fever, bleeding disorders, or a history of seizures.
Adverse Reactions and Monitoring
Common adverse reactions to influenza vaccines include:
- Pain, redness, or swelling at the injection site.
- Fever, chills, or muscle aches.
- Headache or fatigue.
Serious adverse reactions are rare but can include anaphylaxis and Guillain-Barré syndrome. Healthcare professionals should be prepared to manage any adverse reactions.
Vaccine Effectiveness and Surveillance
The effectiveness of influenza vaccines varies from season to season, depending on the match between the vaccine strains and the circulating strains of influenza viruses.
Surveillance systems are essential for monitoring influenza activity and vaccine performance. These systems collect data on influenza cases, hospitalizations, and deaths to assess the impact of vaccination and guide public health interventions.
Communication and Education
Effective communication about influenza vaccination is crucial for increasing vaccine uptake and reducing the burden of influenza. Healthcare professionals should provide clear and accurate information to patients about the benefits and risks of vaccination.
Public education campaigns can also raise awareness about influenza and promote vaccination.
Ethical Considerations

Influenza vaccination raises ethical considerations related to:
- Informed consent: Patients should be fully informed about the benefits and risks of vaccination before they make a decision.
- Patient autonomy: Individuals have the right to make decisions about their own healthcare, including whether or not to get vaccinated.
- Resource allocation: Vaccines are a limited resource, and it is important to prioritize vaccination for those who are most at risk.
Future Directions and Research
Research efforts are ongoing to improve influenza vaccines and vaccination strategies. Areas of focus include:
- Developing universal influenza vaccines that provide protection against a broad range of influenza strains.
- Improving vaccine efficacy in high-risk populations.
- Developing new vaccine delivery methods, such as nasal sprays or patches.
FAQ Resource
What is the target population for seasonal influenza vaccination?
The target population includes individuals at high risk of complications from influenza, such as the elderly, young children, pregnant women, and those with chronic health conditions.
What are the common adverse reactions to influenza vaccines?
Common adverse reactions include soreness at the injection site, mild fever, and muscle aches. These reactions typically resolve within a few days.
How is the effectiveness of influenza vaccines evaluated?
Vaccine effectiveness is assessed through clinical trials and surveillance systems that monitor influenza activity and vaccine performance.